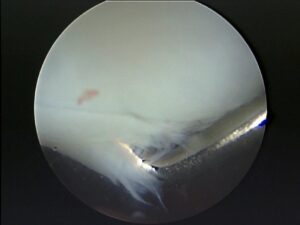
Cartilage Damage
The presence of persistent effusion in a knee being treated for suspected ligament sprain suggests a possibility of Chondral or Meniscal damage.
Chondral defects are common and present in 60% of all knee arthroscopies. Eleven percent of all knee arthroscopies show cartilage defects that may be suitable for cartilage repair procedures (Lars Engebretson). However, the natural history of these lesions and the number of patients that will benefit from a cartilage repair procedure are so far unknown
Diagnosis
The value of arthroscopy for a detailed assessment and grading of a cartilage disorder with regard to definitive planning of a therapeutic procedure cannot be replaced by MRI.
In day-to-day practice, a routine clinical MRI scan has low sensitivity in diagnosing chondral damage when compared with arthroscopic findings. Levy et al reported in 1996 that preoperative MRI scans correctly identified only 21% of the chondral lesions seen at arthroscopic examination (five out of 23 knees in 15 high-calibre soccer players). A prospective study on 190 knees (Figueroa 2007) correlating arthroscopic and MRI scan findings showed that the sensitivity of MRI was 45% with a specificity of 100%. The sensitivity increased with deeper lesions (direct relation with the ICRS classification).
Osteochondral fragments can separate and form a loose body and produce locking.
Classification
Outerbridge Classification
grade 0: normal cartilage
grade I: cartilage with softening and swelling
grade II: a partial-thickness defect with fibrillation or fissures on the surface that do not reach subchondral bone or exceed 1.5 cm in diameter
grade III: fissuring to the level of subchondral bone in an area with a diameter more than 1.5 cm
grade IV: exposed subchondral bone
ICRS Grading
Grade-0:Normal
Grade-1:Nearly normal
Superficial lesions
Soft indentation
Superficial fissures and cracks
Grade 2: Lesions extending down to <50% of cartilage depth
Grade 3: Cartilage defects extending down >50% of cartilage depth as well as down to calcified layer and down to but not through the subchondral bone. Blisters are included in this grade.
Grade 4: Severely abnormal

Radiological Grading
X-Rays
Ahlback grading
- grade 0: joint space not narrowed
- grade 1: joint space narrowed
- grade 2: obliterated <50%
- grade 3 : obliterated >50%
MRI
Radiologically, hyaline cartilage can undergo one of three pathological processes. It can become thinned, thickened or calcify. MRI findings of degenerate cartilage defects typically illustrate obtuse margins and may be associated with corresponding subchondral regions of increased T2-weighted signal reflective of subchondral edema or cysts or low signal intensity reflective of subchondral fibrosis or trabecular sclerosis. The other features of degenerative cartilage disease include cartilage thinning or thickening central and marginal, osteophytes, joint effusion and synovitis.
Traumatic chondral lesions generally manifest on routine clinical MRI as solitary focal cartilage defects with acutely angled margins. The associated alterations in subchondral marrow signal, including bone bruising, bone edema, or subchondral fracture, may be helpful signs in delineating areas of overlying cartilage injury. Traumatic cartilage fragments may remain in situ, become partially detached, or become loose and displace into the joint space. As a result, recognition of a traumatic chondral defect should prompt careful inspection of the joint for a displaced intraarticular chondral body
High-resolution short echo time spectroscopic imaging: Short echo times are essential to see zonal areas of cartilage and are more sensitive for cartilage pathology. This method provides ultra-short echo time, high resolution images of cartilage over a small area, in addition to spectroscopic data. It is possible that this method can be used to distinguish between hyaline and fibrocartilage.
When fat suppression is combined with a 3D spoiled gradient echo sequence, cartilage is the only bright articular structure. However, the 3D spoiled gradient echo sequence with fat suppression has the highest reported accuracy rate for the detection of hyaline cartilage abnormalities Delayed gadolinium enhanced MRI of cartilage (dGEMRIC) has recently been proposed as a means of measuring glycosaminoglycan concentration. Using this technique, T1 values are directly related to GAG concentration within cartilage. This may be a useful imaging tool to monitor osteochondral grafts and chondrocyte implants.
References
- Aroen A, Loken S, Heir S, Alvik E, Ekeland A, Granlund OG, Engebretsen L. Articular cartilage lesions in 993 consecutive knee arthroscopies.
- Hjelle K, Solheim E, Strand T, Muri R, Brittberg M. Articular cartilage defects in 1,000 knee arthroscopies.Arthroscopy. 2002 Sep;18(7):730-4.
- Widuchowski W, Widuchowski J, Trzaska T. Articular cartilage defects: study of 25,124 knee arthroscopies.Knee. 2007 Jun;14(3):177-82.
- Levy AS, Lohnes J, Sculley S, LeCroy M, Garrett W. Chondral delamination of the knee in soccer players. Am J Sports Med 1996; 24(5):634-9.
- Figueroa D, Calvo R, Vaisman A, Carrasco MA, Moraga C, Delgado I.Knee chondral lesions: incidence and correlation between arthroscopic and magnetic resonance findings.Arthroscopy. 2007 Mar;23(3):312-5.
- Outerbridge RE. The aetiology of chondromalacia patellae. J Bone Joint Surg [Br] 1961;43-B:752-7.
- Ahlbach S: Osteoarthrosis of the knee: A radiologic investigation. Acta Radiol 227(Suppl):S7, 1968
- von Engelhardt LV, Kraft CN, Pennekamp PH, Schild HH, Schmitz A, von Falkenhausen M. The evaluation of articular cartilage lesions of the knee with a 3-Tesla magnet.Arthroscopy. 2007 May;23(5):496-502.
- Kneeland JB. MR imaging of articular cartilage and of cartilage degeneration. In: Stoller DW. Magnetic Resonance Imaging in Orthopaedic & Sports Medicine. CD-ROM. Lippincott-Raven Publishers, 1997.
